A study by University of Manchester epidemiologists is the first to show stark differences in opioid prescribing by GPs in areas just a few miles apart.
The study of English data in the journal Epidemiology and Communality Health, shows how people in our towns and cities divided by deprivation are also divided by opioid use.
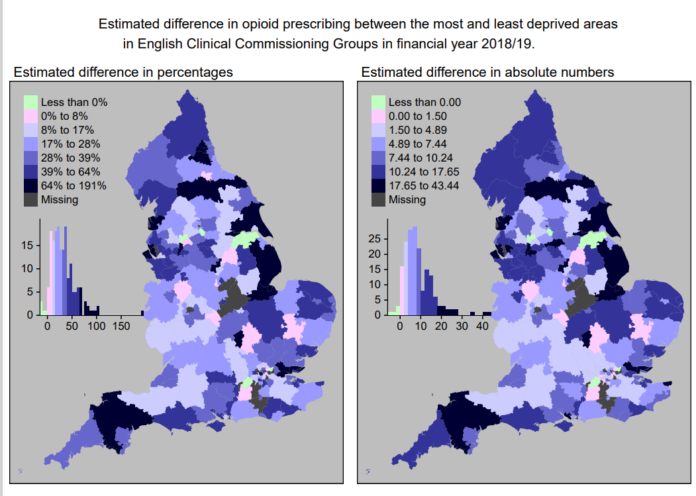
Lincolnshire East was the most unequal clinical commissioning group area in England: the level of prescribing for most deprived areas was twice as much as those in the least deprived areas. It contrasts markedly with nearby Lincolnshire North.
They also showed that prescribing in the most deprived areas in North England was 1.2 times higher than the national average for areas with similar deprivation levels and 3.3 times higher than the most deprived areas in London.
Prescribing in the most deprived areas was substantially higher than the least deprived areas. On average it was 9.70 Defined Daily Doses/1000 people/day higher.
Meanwhile in the most unequal Clinical Commissioning Group area, prescribing in the most deprived areas was twice that of the least deprived areas.
Led by PhD researcher Magdalena Nowakowska, the team used sophisticated statistical analysis linking different datasets to observe GP prescribing in 32,844 geographical units, each representing an average of 1,500 people in England, across 195 CCG areas.
Deaths from overdosing and dependency on the class of drugs which include Fentanyl, Morphine, Oxycodone, Tramadol and Codeine have risen dramatically in the West over the past two decades.
Though researchers and policy makers know that prescribing is associated with higher deprivation levels, this is the first time the patterns of this relationship across the country have been fully mapped.
East and South Lincolnshire, Fylde and Wyre, East Riding and the Wirral were the top five CCG areas with the biggest differences in prescribing.
Significant differences in prescribing within CCGs may suggest that policies and interventions at a smaller level, addressing specific communities may be needed.
However, say the team, the observed variations in opioid prescribing may reflect wider issues with social, economic and health inequalities which also need to be addressed.
“Much is known about increasing opioid prescribing and opioid-related deaths, but this study adds greater understanding of its association with deprivation”, said Professor Evan Kontopantelis, from The University of Manchester
Magdalena Nowakowska said: “Knowing where exactly which populations are being prescribed more is a powerful way to guide policy responses and interventions so they can allocate resources to areas with highest levels of opioid prescribing.”
“CCG areas have populations of 100,000 to 500,000 people, so these large units can’t really describe the experience of the people who live there.”
“However, the smaller units we used, using some novel methodological approaches and datasets, can give a more accurate picture – which can be incredibly useful for policy makers.”
The team measured opioid prescribing in Defined Daily Dose, a statistical measure devised by the World Health Organisation which allows researchers to compare drug usage between different environments.
They modelled the effect of socioeconomic deprivation on opioid prescribing controlling for population demographics and the prevalence of specific health conditions using data from 2018 and 2019.
The Index of multiple deprivation used by the team is recognised as an accurate measure, and uses health, public services, education, crime, and other factors.
She added: “Though we didn’t look specifically at why there are such stark differences within relatively small geographical areas, people living in more deprived areas are more likely to experience more complex health needs and poorer access to alternatives for opioids are likely to help explain the disparities.”